Abstract
Background: Adequate reconstruction of the soft palate to achieve quality of phonation is one of the main objectives of cleft palate repair. Even with adequate repair, the soft palate may remain short, leading to Velopharyngeal Insufficiency. In such cases lengthening is achieved by sacrificing other important anatomical structures.
Objective: We present a new technique in the reconstruction of the soft palate that elongates it in an efficient way providing adequate sufficiency and uvular competence, without sacrificing other palatal structures.
Methods: During a five-year period, this technique was applied to a total of 731 patients, 437 in primary repairs and 294 in secondary or revision cases. All patients were subjected to a quantitative analysis with the «Alvarez Scale» or Speech Score both before and after surgery.
Results: There was a notable improvement in our series in the prevention and treatment of Velopharyngeal insufficiency (VPI). There was a gain of one to two points (over fifteen) in improvement as compared to what the revision group had in their preoperative evaluation.
Conclusion: In our experience, the Third Generation Veloplasty (TGV) is more effective in improving the velopharyngeal function than the first generation Veloplasty (OR = 2.76)
Keywords | Velopharyngeal insufficiency (VPI), First Generation Veloplasty (FGV), Second Generation Veloplasty (SGV), Third Generation Veloplasty (TGV), Uvular insufficiency (UI), Uvular incompetence (UIc), Speech Score (SS)
Received | 22-07-2020: Accepted | 25-09-2020
Corresponding Author | Edwar Alvarez MD
Email: edwaralvarezc@hotmail.com
Introduction
From the beginning of palatal reconstruction, surgeons sought the three-layered anatomical reconstruction of the congenital defect between the 1,2 oral and nasal cavities. This fundamental principle in the repair of the cleft palate has not changed since Bernard von Langenbeck.
With respect to the bony palate, the reconstruction has evolved in the form of wide dissection techniques, such as Veau-Wardill and Bardach. Current methods also include conservative techniques with minimal incisions that have taught us to temper surgical procedures by dissecting what is strictly necessary to achieve repair of the defect with minimal scars. We have described these as the Surgical Philosophy of the 3,4,5 Palate, or cut as you go. These methods have shown encouraging results, however, they have a long learning curve.
Despite adequate closure of the palatal cleft, speech disorders are quite common in these patients. Hence, there is a need to look for reconstructive alternatives 6,7,8 in order to improve functional results.
To understand the cleft palate malformation, it is important to relate the pathology with anatomical
Speech samples were recorded for all patients pro- operatively, as well as post-operatively. Speech assessment was done using the Alvarez score. The primary cases had at least a 3-year follow-up, and the secondary cases had a one-year follow-up. The results of this technique were compared to that of a ‘control group’, comprising of patients who under- went first generation veloplasty (intravelar veloplasty method), before we started implementing the current technique
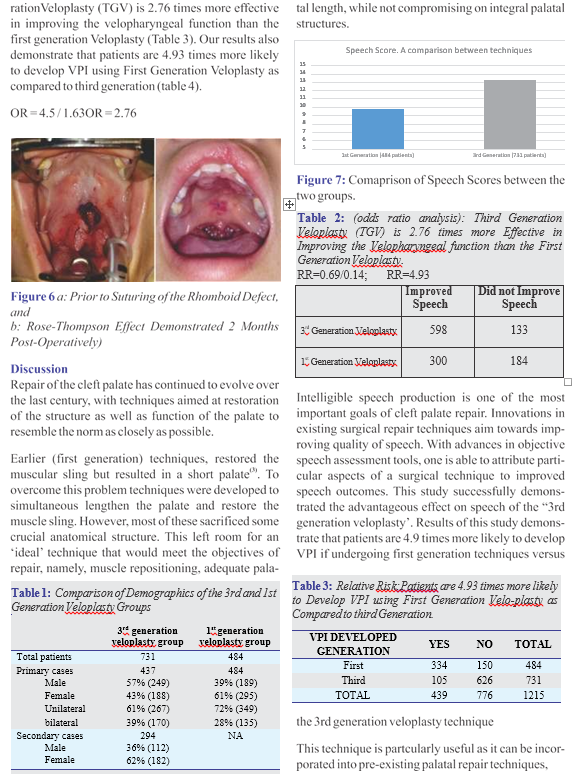
The relative risk was calculated, for development of VPI with first generation technique versus third generation technique. The odds ratio for improve- ment of VPI with third generation technique was also calculated.
Surgical Technique
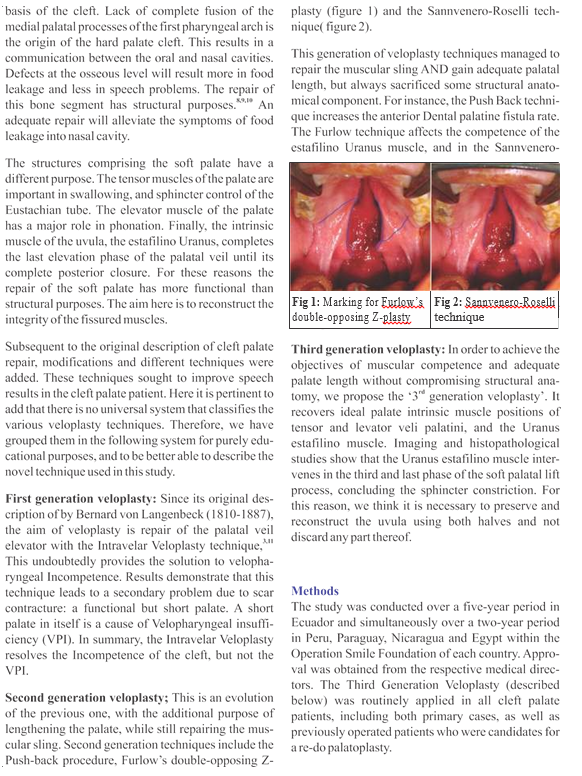
With the patient in Rose’s position and a Dingmann mouthpiece in place, the soft palate was infiltrated with a solution containing 0.25 mg of bupivacaine and epinephrine 1: 100,000. After waiting for a laten- cy period of seven to ten minutes, de-epithelialization along the medial border of the cleft uvula was done on both sides, as shown in figure 3.
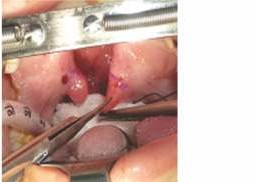

Figure 4: A full thickness, 1 cm Long Cut made Parallel to the Posterior Border of the Uvula
Once this step is done, fibers of the Uranus estafilino muscle can be clearly seen from the base of the uvula. After that a full thickness cut that involves the oral mucosa, uvular muscle and nasal mucosa has to be made; the path and direction of this cut will be parallel to the posterior border of the uvula no further than one centimeter as shown in Fig. 4.
Once this cut is made on both sides, that is to say on each palate hemi-veil, the remaining uvulas are push- ed towards the posterior pharyngeal wall forming a rhombus. This defect is closed in the midline with absorbable vicryl 6/0 sutures.
With consequent suturing of this rhombus, there are two effects: firstly the contact surface of the elevator and Uranus estafilino muscles increases, ensuring adequate competence. Secondly, through the Rose- Thompson effect there is elongation of the soft palate. (Figure 5 and 6)

Figure 5: Creation of Rhomboid Defect
Results
A total of 731 patients were treated with the third generation veloplasty technique. The control group included a total of 484 cases, treated with Intravelar Veloplasty technique (First Generation Veloplasty). The details of both these groups are elaborated in Table 1. The phono-audiological follow-up during three post-operative years in primary cases and one postope-rative year in secondary review cases detected a two-point improvement in the Alvarez speech score (Table 2).
The odds ratio analysis shows that the Third Gene
without any added morbidity as it does not sacrifice other anatomically important structures of the palate where important modulations of sounds for speech are made.
Conclusions
The Third Generation Veloplasty concept has allowed us to teach our residents the logical objectives of Soft Palate repair, which are adequate length and motor capacity. This also highlighted the importance of the estafilano uranus muscle in the final part of the palatal lift process.
The Speech Scale proposed by us serves as an auxi- liary mechanism to evaluate the effect of the muscular repairing technique.
This technique has provided us with a new way of performing Veloplasty, which can be integrated to any other previous technique. Nevertheless, larger multicentric studies to further evaluate the results of this technique are required.
Acknowledgments:
Dr. J. Núñez, Operation Smile Peru
Dr. M Fariña, Operation Smile Paraguay Dr. R. Cabrera, Operation Smile Nicaragua Dr. F. Córdova, Operation Smile Ecuador Dr. Ghulam Qadir Fayyaz-Pakistan
References
- Murray J. Report of a Clinical Standard Advisory Committee (CSAG) on Cleft Lip and/or Palate (Uni- ted Kingdom). London: Her Majesty’s Stationery Officer. 1998.
- Shaw WC, Dahl E, Asher-Mcdade C, Brattström V, Mars M, Mcwilliam J, Mølsted K, Plint DA, Prahl- Andersen B, Roberts C, Semb G. A six-center inter- national study of treatment outcome in patients with
clefts of the lip and palate: Part 5. General discussion and conclusions. The Cleft palate-craniofacial jour- nal. 1992 Sep;29(5):413-8.
- Perko M. The history of treatment of cleft lip and palate. InHistorical Aspects of Pediatric Surgery 1986 (pp. 238-251). Springer, Berlin, Heidelberg.
- Larossa D. The state of the art in cleft palate surgery. The Cleft palate-craniofacial journal. 2000 May; 37(3): 225-8.
- Strong EB, Buckmiller LM. Management of the cleft palate. Facial plastic surgery clinics of North Ameri- ca. 2001 Feb 1;9(1):15-25.
- Van Lierde KM, Monstrey S, Bonte K, Van Cauwen- berge P, Vinck B. The long-term speech outcome in Flemish young adults after two different types of palatoplasty. International journal of pediatric otorhi- nolaryngology. 2004 Jul 1;68(7):865-75.
- Bae YC, Kim JH, Lee J, Hwang SM, Kim SS. Com- parative study of the extent of palatal lengthening by different methods. Annals of plastic surgery. 2002 Apr 1;48(4):359-64.
- Agrawal K. Cleft palate repair and variations. Indian journal of plastic surgery: official publication of the Association of Plastic Surgeons of India. 2009 Oct; 42(Suppl):S102.
- Noordhoff MS, Kuo J, Cheng WS. Results of the Widmaier-Perko palatoplasty in clefts of secondary palate. Annals of the Academy of Medicine, Singa- pore. 1983 Apr;12(2 Suppl):359.
- Leenstra TS, Kohama GI, Kuijpers-Jagtman AM, Freihofer HP. Supraperiosteal flap technique versus mucoperiosteal flap technique in cleft palate surgery. The Cleft palate-craniofacial journal. 1996 Nov; 33(6): 501-6.
- Andrades P, Espinosa-de-los-Monteros A, Shell IV DH, Thurston TE, Fowler JS, Xavier ST, Ray PD, Grant III JH. The importance of radical intravelar veloplasty during two-flap palatoplasty. Plastic and reconstructive surgery. 2008 Oct 1;122(4):1121-30.

